For Rukmini, a daily wager working on a construction site in Kundsebara village in Kashipur, Uttrakhand, life was already tough. Her daughters were still in school, while her husband, Ram Singh, was struggling to make ends meet as a farmer. One day, while returning home, Rukmini fell unconscious. The local medic could not ascribe the root cause, and passed it off as fatigue.
Now think about how this case could be treated in the past, present and future:
In the 1990s, the village did not have any specialised medical amenities for testing and diagnosing. Rukmini would either have been brought back home and have received no scientific treatment. Or she would have had to travel to Delhi for treatment — which would have meant additional expenditure. Also, she might have had to travel down to the hospital each time a follow-up was required, in the process taking the treatment cost several notches higher.
Cut to 2019, Rukmini and her family don’t have to worry about the lack of a specialist in their area. Thanks to telemedicine, doctors located in cities can ably treat patients in any location. So Rukmini can walk into an e-clinic and connect to a specialist through audio or video conference. These clinics can also conduct a host of tests including ECG, pulse and heartbeats reading. The doctor then suggests the further course of action — either prescribes medicines or advises more detailed tests. The blood samples of these tests can be transported with the help of drones — to save time — and results interpreted through artificial intelligence (AI) and machine learning (ML) systems. E-consultation has been made much cheaper by start-ups, through tie-ups with various hospitals and state governments.
Move forward to 2029. Now, Rukmini would visit a kiosk located in the village, which would be an AI-powered unmanned clinic. It would provide Rukmini video consultation with a doctor, dispense medicines based on the prescription and also run basic blood tests. If the case is found to be serious, then the doctor might recommend the patient to visit the nearest hospital for further treatment. Or, who knows, a robodoc deployed at the village and controlled remotely by a specialist may take it forward.
While the impact health tech can create in rural areas is huge, its efficacy is not lost in the urban regions as well. Take for instance Pooja, a 29-year-old working professional. It had been just a year since her marriage to Karan, who is also employed in a private-sector company. All was going well until Pooja started falling ill constantly. Sometimes it was fever, sometimes a bad stomach, and sometimes a headache. She also began losing weight, at which point they realised that they need to consult a specialist. A few years ago, in such a situation, there would have been absolute confusion over which hospital to go to or which doctor to consult. Then, of course, Pooja would have had to go through multiple tests before the doctors could finally ascertain her illness and start treatment. Today, this has been made much simpler. Pooja can log on to an app which aggregates doctors across different specialties. The AI and ML integrated into the app will analyse Pooja’s case and give her the most relevant doctors in her vicinity. She can then go through the list, check their ratings and set up an appointment. It’s as simple as ordering a biryani through Zomato. Meanwhile, at the doctor’s end, he will have access to Pooja’s digitised medical records so that, before he meets her, he has her complete history on a dashboard. In case tests are conducted, for instance an EEG or CT scan or MRI, the results are read with the help of sophisticated programming, which also improves precision of diagnosis.
The future is unimaginable. But at the very least, in a few years, everyone will be walking around with wearables, just the way you see people with handsets and headsets. Wearables would be constantly, yet non-intrusively, monitoring vitals — blood sugar, heart rate, breathing — and create an alert on any irregularities on the same. An alert would also be sent to the care giver and the doctor. Any problem would be tackled at the first step, reducing both cost and time taken for treatment.
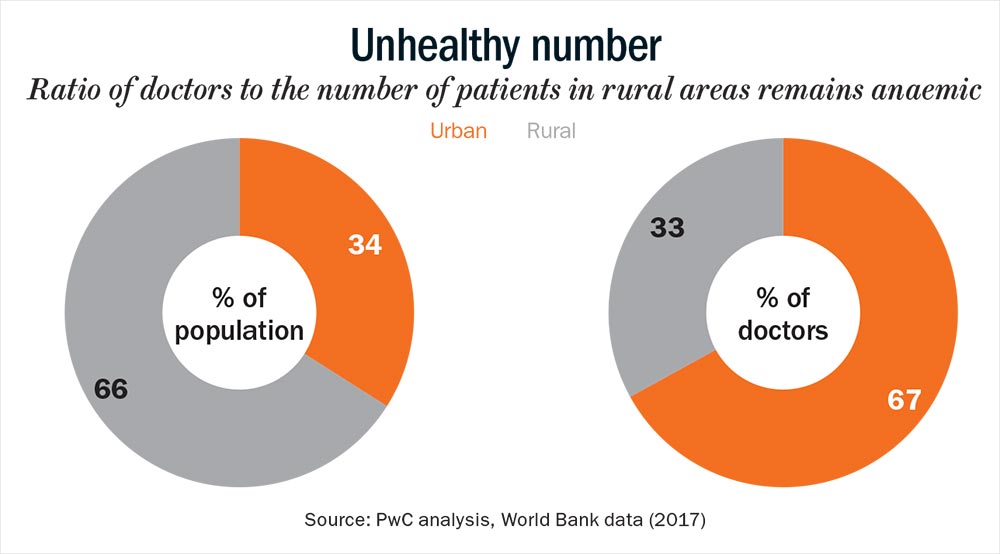
Technology is changing everything around us, including healthcare. And it’s required, especially in a country like India. As PwC notes in a recent report, “Uberisation of the healthcare industry is required to radically change the way healthcare operates.” Rahul Guha, partner and MD, Boston Consulting Group India, agrees and adds, “Tech adoption in Indian healthcare will be faster than in other markets, because the capacity constraint is so severe that technology has to be a mediator.”
So how exactly are start-ups leveraging technology? Simply put, there are three main uses of technology in healthcare: Improve accessibility and affordability, delegate diagnostics to ML, and AI and thirdly, move towards connected healthcare.
Tele tech
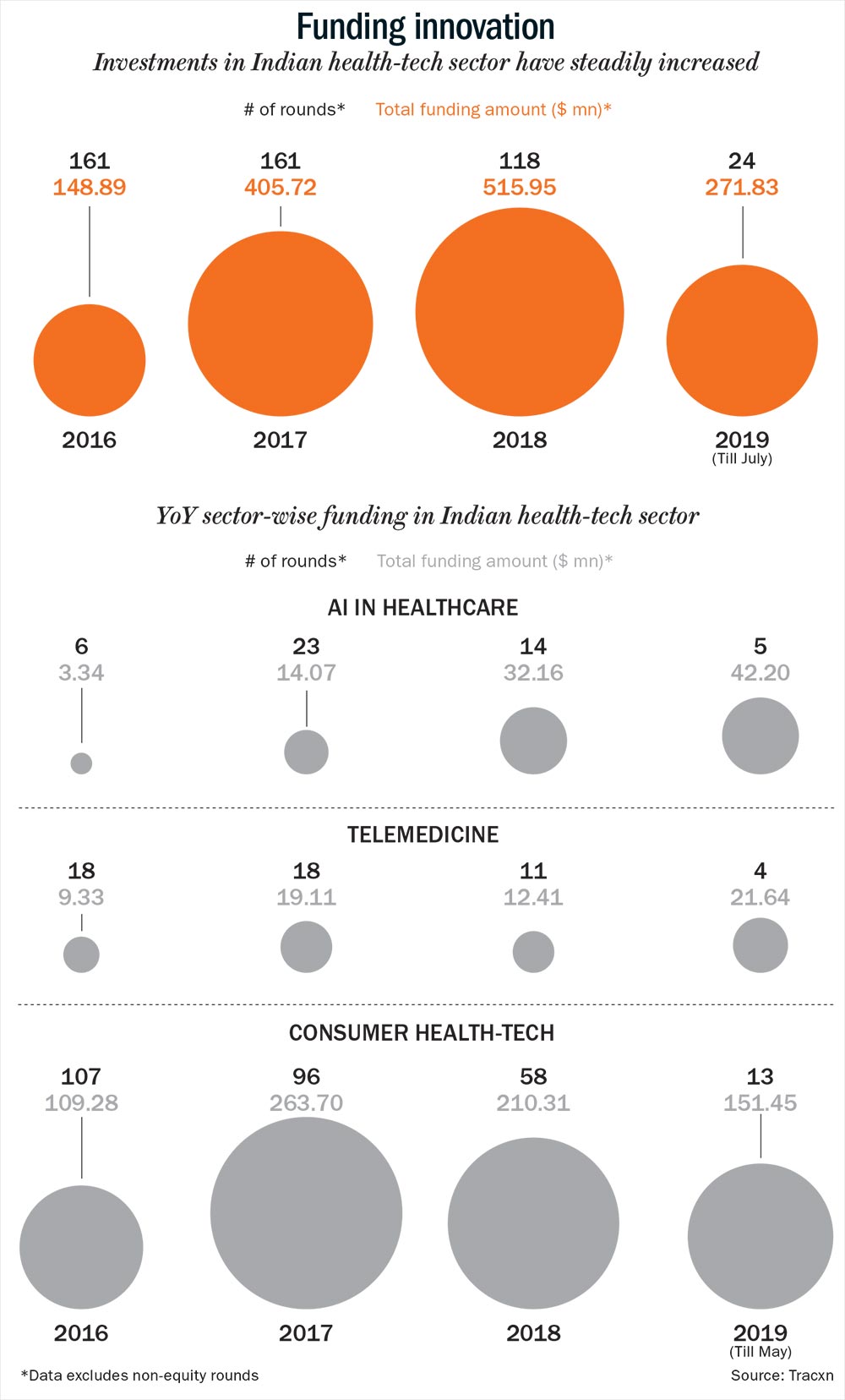
In India, access to quality healthcare is the biggest problem, primarily because of a skewed doctor-patient ratio and insufficient healthcare infrastructure (See: Unhealthy number). However, Sendil Kumar, a veteran healthcare IT specialist and founder of med-tech firm, Csoft Technology, says that technology can be the saviour. And a bunch of start-ups are already leading the way in this field, thanks to the rise in funding as well. (See: Funding innovation) “The need to go to a clinic itself is slowly disappearing. Mobile consultation will become more widely adopted especially in rural areas due to low-cost data plans and cheap smart phones,” points out Kumar.
This has been made possible through telemedicine. Take for instance Tattvan, which operates five e-clinics across India. These clinics are equipped with a machine resembling an ATM machine, and have a doctor and nurse stationed there. Once a patient walks in, they help him connect to a specialist through videoconference organised through FDA-approved Twilio, a cloud communications platform. “The machine is equipped with a telemedicine kit, that is, devices that run on bluetooth. The stethoscope works in low frequency and the oscillation can be heard by doctor located several kilometres away in the city,” explains Ayush Mishra, co-founder, Tattvan. The e-clinic has devices to diagnose dengue, malaria and other diseases, without the need to travel to a city hospital. Medication prescribed is then either supplied at the clinic or sent across by the doctor.
Beyond cheaper consultation and saving travel time, the clinic helps in timely diagnostics and saving life. Mishra says that a girl had developed lumps around her chest. One of the local doctors in the area said she has breast cancer and advised her to start chemo. Devastated on hearing this, her family brought her to the e-clinic for a second opinion. Fortunately, after looking at her reports, the gynaecologist concluded that the lumps were benign. “If the specialist hadn’t been consulted, the girl would have ended up taking chemotherapy, which would have led to a host of side effects,” says Mishra.
Then there is MedCords, which provides telemedicine at a cheaper cost. It encourages people in rural areas to digitise their health records and helps them connect to a city-based specialist through an app. “We started with treatment for diseases such as fever, headache, cough, cold and now solve about 23 ailments including anxiety, loose motions and joint pains,” says Shreyans Mehta, co-founder, MedCords. The consultation fee is Rs.99 and the service has been extended to 2,300 villages across five districts in Rajasthan.
Much like the start-ups, bigger firms too are leveraging telemedicine to provide medical aid to patients in critical state. Vikram Damodaran, chief innovation officer of GE Healthcare, says that they introduced a tele-ICU service a few years ago, where one ‘intensivist’ at a command center could manage hundreds of ICU beds. The solution, called CritiNext, has been rolled out by Fortis in partnership with GE Healthcare. These e-ICUs use electronic medical records, audio-visuals and smart alert system as rapid response tools to provide non-stop monitoring, assessment, support and interventional services. Currently, they remotely manage over 150 ICU beds in cities such as Amritsar, Dehradun, Raigarh and Khulna (in Bangladesh), from Delhi, treating over 500 critical patients every month.
Seeing the potential in telemedicine, both MedCords and Tattvan are now looking at increasing their footprint. While MedCords plans to remain focused on rural areas, Tattvan has already opened a clinic in Kabul and is now planning to open more in Iraq, Ethiopia, Uzbekistan, Maldives as well as in Delhi and Gurugram.
Intelligent care
While telemedicine is the first step, it has to be complimented by mass adoption of AI and ML to provide accurate diagnostics. An example of this would be, Qure.ai, which uses AI to assist radiologists with reading X-rays, scans and generating reports. Its algorithm is deployed as software in the X-ray, CT scan or MRI machines, leading to faster and cheaper diagnosis.
“We wanted to automate X-Ray reading with the help of AI. This will make the radiologist more productive, accurate and save time for the patient,” says Prashant Warier, who co-founded the firm in 2016. With Qure.ai’s solution, what used to take weeks to diagnose is investigated now in less than five minutes. They have successfully reduced the time taken to diagnose a person with tuberculosis, from five weeks to a day, in Philippines.
Early diagnosis, in fact, is a crucial factor in the treatment process. This is where a start-up like Niramai fits in. The Bengaluru-based start-up specialises in detecting breast cancer at a much earlier stage than traditional methods. “In breast cancer, the most common test used globally, is mammography. But it doesn’t work on women under 45 years of age. Thus, we developed a novel and disruptive tool by using AI and ML technology to provide early detection, which works for women of all age groups. We just measure the temperature variations in the chest, and our AI algorithms analyse it and generate a breast health report,” says Dr Geetha Manjunath, co-founder, CEO and CTO of Niramai. While a mammogram costs around Rs.3,500 per screening, Niramai’s test is priced at Rs.1,500. About 7,500 people have been screened by Niramai’s solution, deployed across 30 locations in 10 cities in India.
AI and ML are also being utilised for innovative use-cases such as dispensing medicines. Caredose, co-founded by Gauri Angrish, has created ‘DoseDroid’, which is an automated multi-dose packaging robot. On receiving an order, the robot cuts medicines into unit pills, sorts and pouches medicines according to prescribed doses, labels each dose pouch and tracks manufactures’ information. What’s more, there is a smart attachment on the dispenser, which beeps if the patient does not tear the pouch of dosage at the stipulated time. An alert can also be sent to caregiver and doctor, so that they can remind the patient to take the medicines. A person just needs to log on to the platform, upload prescription and place the order to receive the carefully segregated dosages.
“Non-adherence to prescription leads to more complications, and we want to help patients avoid this situation,” says Angrish, who is also the CEO. The start-up has partnered with medical firms such as Apollo Pharmacy, Clinton Health Access Initiative and Max Healthcare to source medicines. So the next time you forget to take medicines on time and end up with an uncomplimentary blood test result, you can no longer feign innocence. The doctor will know exactly which doses you missed taking!
Since food habits also play a pivotal role in ensuring holistic well-being of a person, apps such as HealthifyMe have seen a huge success. Founded by Tushar Vashisht, this app offers an automated yet curated diet plan based on 350,000 pre-designed meals and a user’s preferences, local cuisine nuances, weight-loss goals and medical conditions. HealthifyMe also has a chat-bot Ria that helps people identify unhealthy food such as veg mayo sandwich, kachoris and samosas and suggests healthier replacements such as roasted kala chana, tomato soup and besan cheela. “The app has helped consumers achieve their fitness goals and reverse severe health conditions such as diabetes, hypertension, PCOD, and PCOS,” says Vashisht.
Stay connected
While multiple start-ups are offering niche services, the cherry on the cake would be when these different layers of services come together.
This is the future Nilesh Jain is building his platform, Clinivantage, towards. It essentially connects all the “connected devices” onto one platform to provide a seamless treatment for the patient and improved database for the doctor. Jain, director and co-founder of the start-up, points out how healthcare has evolved. About twenty years ago, the ECG machine was as big as a three-seater sofa. Today, it has become as small as a phone, and in the future, it could well become a wearable. Similarly, fifteen years ago, one had to go to the lab for a blood test. That changed with the launch of devices such as One Touch and Abbott’s blood-glucose monitor. Soon, there could be a non-intrusive monitor for every person to alert him about his blood glucose level and enable him to make informed food choices. It will also enable doctors to continuously monitor the effectiveness of a drug on a patient instead of waiting for longer duration. “Such progress will make healthcare much more capable and integrated. Slowly, healthcare will transform into wellness industry than into reactive, episodic care,” he explains.
“Our platform is cloud based. We connect IoT devices in healthcare — from ICU and blood pressure monitors to urine analysers,” says Jain. This helps create a complete ecosystem for start-ups across the spectrum of healthcare, including application of AI and ML for critical tests and treating diabetes, nephrology and cardiac disorders, CPOD, substance abuse and TB.
Further, he adds that their solution also comes in handy in post-operative care. “The doctors keep you in the ICU for additional days just to keep track of your vitals. Instead, we can shift ICU to your home. Today it is not rocket science to provide the same care at home with a few small devices costing about Rs.3,000. Thus, we not just create extra capacity in ICUs, but also reduce the overall cost of episode,” he says. Their solution — connected devices and access to their platform through mobile/iPad or a smart device — has been deployed in six countries across 500 hospital beds and have served over 13 million consumers already.
HealthAssure too is viewing connected healthcare as the way forward to the evolution of med-tech in India. It aggregates primary healthcare services such as medical centres, hospitals and doctors, and helps patients connect with the right doctor based on their location and ailment. Ankush Chatterjee, director and head of the consumer business unit, HealthAssure states that they have also standardised the fees charged, which is always at a 50-60% discount compared to market. It is also developing a direct-to-consumer route by working with corporate and medical institutions.
Taking connected healthcare a step further is medECUBE, which helps in clinical coordination by plugging loopholes. It has six verticals, each serving a unique need, ranging from assisted healthcare monitoring and planning to helping specialists guide local doctors through telemedicine.
Citing an example of their service for senior citizens, Dr Dilpreet Brar, founder and MD, medECUBE, states that one of their clients is a 90-year-old man staying in Delhi’s Som Vihar. “The day he subscribed, we took note of his entire medical history and planned his diagnostics accordingly. Whenever he falls sick, he just has to call me and the entire logistics is taken care of by us. His children stay abroad and thus, a service such as ours is of great value to him,” she explains.
The company is now looking to ramp up its services to include teleradiology, telepathology and telegenetics. “We are looking to build a command centre wherein a test can be done in any part of the world and uploaded on the platform, where it can be read by a specialist,” she adds.
There are also services such as DaytoDay, which help patients prepare for surgery and recovery. “Most of the healthcare happens out of hospital walls. A patient’s body goes through a lot of change post surgery and before it. While people get good support in hospitals, it is their journey before and after that needs to be taken care of, and this is the problem we wish to solve,” says the start-up founder Prem Sharma. DaytoDay currently manages open-heart surgery and complex surgery patients for Fortis.
So what exactly do they “manage”? Well, when a patient signs up on the app, they are informed about the surgery, how to prepare for it, how to control blood sugar, and given psychological support. After surgery, the app continues the guidance of delivering personalised care, which one can’t find on Google. “We are also moving into cancer care, where currently, the tumour is treated, but the patient is psychologically affected,” adds Sharma.
Journey ahead
At present, there is an obvious exuberance around the use of technologies in the healthcare industry. But with time, it is expected to move from being a novelty to being an essential part of India’s healthcare ecosystem. Damodaran says that the biggest challenge in India is the country’s “inverted pyramid of care”. In an evolved society, a large number of patients (the bottom of the pyramid) are first directed to primary care. The patient is then promoted to secondary and tertiary care only if the illness is acute. “In India, patients promote themselves into the tertiary care setting, even if it is for a general check-up, thus choking the tertiary care system,” he says.
Jain of Clinivantage says that we are likely to see a major transformation in the next ten years. “We will see a lot more connected devices to aid diagnosis and treatment at lower costs,” he says, adding that ‘homecare’ that is treating the patient at home through non-intrusive, remote monitoring, will see a huge adoption.
With rapid adoption of technology and clear intent from all stakeholders, the healthcare industry in India is at the cusp of a major transformation. The 2029 healthcare scenarios for Rukmini and Pooja are not a distant dream, but a plausible reality. How it takes shape depends on continued efforts as well as faster deployment and lowered pricing. But going by the current pace of innovation, it doesn’t seem long before healthcare will be made available at the tap of a finger, literally.